Hemorrhoids - a disease associated with varicose inflammation and swelling of the veins of the rectum in the anus. Affected areas protrude from the outside, can form large nodules (lumps) that interfere with the promotion and release of feces. The disease affects men and women, it is dangerous for the rupture of veins, the addition of a secondary infection.
Classification of hemorrhoids
Depending on the location of the pathological site, 2 types of disease are distinguished:
- Outer. The veins in the anus, which are covered with skin, become inflamed. Because of this, it is more difficult to damage the affected areas, they have a stronger "protection". Discomfort during defecation is less, but often unpleasant friction is created by the linen. Complications of external hemorrhoids occur less frequently, it is easier to treat.
- Interior. The affected veins are located in the rectum above the anus, making it difficult to determine the early stage of the disease. The vessels are covered with a thin epithelium, therefore they are more susceptible to mechanical damage. The internal form of the disease often becomes chronic, it is more dangerous with complications, it is more difficult to treat.
According to the severity of the course, internal hemorrhoids are divided into 3 stages (stages):
- Beginners (1). The joints come out, bleed, but do not fall.
- Moderate (2). With muscle tension (during defecation, exercise), swollen veins come out of the anus. When everything calms down, they come back.
- Heavy (3). The joints fall, even when there is no muscle tension, they do not pull.
Symptoms
The main signs of hemorrhoids are bleeding from the anus, tension pain in the muscles of the rectum. The complete picture depends on the stage of the disease. If nodules appear (swollen separate sections of veins), they look like lumps of a dark pink or purple color (rarely almost black), are easily palpable, and feel dense. The shadow depends on the filling of the vessels: if blood clots have formed, the blood has collected and cannot come out, the nodes will be dark.
internal hemorrhoids
In the first days and weeks, the disease almost does not appear. It starts with edema, which is not felt unless you start examining the rectum from the inside. There are no pain receptors in that part, so a person does not experience discomfort, even during the defecation process.
At an early stage of hemorrhoids, you can learn of its existence only with blood droplets appearing after the release of large and strong stools. Due to edema, the walls of the rectum narrow the lumen, the mucosa is damaged more during constipation. Important - with hemorrhoids, almost any bowel movement will cause the appearance of a small amount of blood.
Other symptoms will follow:
- Pain during bowel movements. Severe swelling will provoke muscle spasms, so even soft stools will cause discomfort.
- Burning, itching. Due to inflammation in the rectum, a lot of mucus is formed, which irritates the tissues.
- Blood. Appears in large numbers when nodes are formed. Important: with hemorrhoids, it is bright red - not dark.
- drop joints. They appear in the last stages of hemorrhoids. First, they pull themselves together, then they have to be "pushed" with the finger.
Outer
The external veins are covered with skin, which has many pain receptors. Already at an early stage of hemorrhoids, a person will experience discomfort if the vessels are swollen. The pain appears during defecation, and during rubbing of the anus, and with close contact of the linen with the skin. If the inflammation is severe or a blood clot forms in the vein, a large lump forms. It is easy to touch, touching causes pain.
The skin with external hemorrhoids becomes sensitive, often gathering in folds due to swelling. The process of cleaning the anus after defecation is difficult, so the risk of secondary infections increases. Subsequently, blood appears if the hemorrhoids are damaged, but there will be less than with the formation of internal cones.
Causes
The disease is associated with impaired blood flow to the veins of the rectum, which is often caused by overload in the pelvic organs. Due to them the pressure in the veins increases, which swell and come out. In most people, this happens due to improper lifestyle and nutrition, but doctors do not rule out the influence of heredity, genetic vascular abnormalities and increased blood clotting.
Possible reasons why hemorrhoids appear:
- Frequent constipation - leads to tension of the anal veins, damage to the mucosa during the promotion of solid feces.
- Diarrhea - acute and chronic.
- Pregnancy - causes swelling, provokes increased pressure from the uterus into the rectum.
- Hormonal fluctuations - provoke atony of the muscles of the pelvic organs.
- Intestinal oncology (most often - colon).
- Delayed operations on the rectum, less often - on the pelvic organs.
- Spinal cord injury, spinal curvature, lower back injuries, sacrum, coccyx.
Additional risk factors:
- Sedentary lifestyle - causes blood stagnation in the pelvis.
- A low-calorie, low-fiber diet causes constipation.
- Lifting weights causes muscle tension.
Diagnosing
The doctor reviews the medical history and asks explanatory questions to rule out other causes of bleeding from the anus. Hemorrhoids are similar in symptoms to tumors in the digestive tract, polyps, anal fissures, mucosal prolapse.
After the doctor performs a rectal examination, feeling the lower part of the rectum with the finger. At an early stage of internal hemorrhoids, this may not yield results, and at a later stage, the procedure will be postponed if the swelling is very severe and touching the patient causes acute pain. To clarify the diagnosis and a more detailed examination of the anus, examinations are performed by a surgeon or a gastroenterologist.
The following methods are applied:
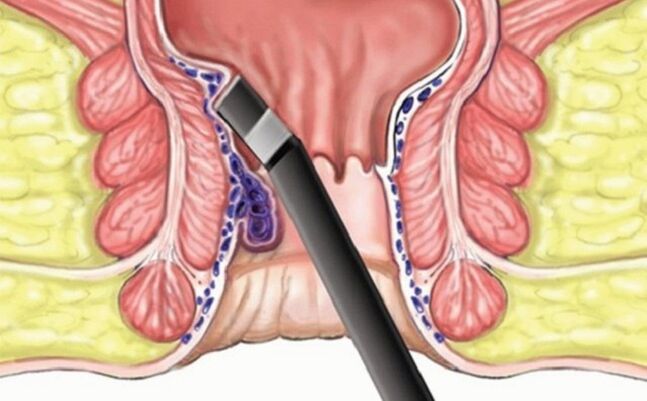
- Anoscopy. Inspection of a rectal section up to 10 cm long from the anus. The procedure is painless, but some patients are given local anesthesia (gel, spray).
- Sigmoidoscopy, colonoscopy. A tube is inserted into the patient's colon to rule out other causes of bleeding (tumors) and suspected lesions in the upper extremities.
- MRI. Tomography is done if it is not possible to make an accurate diagnosis based on other procedures.
Laboratory research
Blood tests are rarely prescribed, it depends on the clinical picture of the disease. This is necessary if a secondary infection has occurred to determine the pathogen. They also do an analysis in situations where bleeding from the rectum is abundant to look at the hemoglobin level, number and activity of red blood cells. The main diagnosis does not require laboratory procedures.
Treatment
If there are no symptoms of the disease, no special therapy is needed. The doctor will advise you to change your lifestyle and diet so that hemorrhoids do not develop, the stool becomes softer and does not damage the inflamed or swollen mucosa. The patient will be offered to move more, do gymnastics that aims to work the muscles of the "lower press" and the pelvis.
How to treat hemorrhoids, which cause discomfort, is determined by the doctor, taking into account the stage of the disease. In the early stages, it is really possible to manage only with medication. If there are many nodules, they thrombosis and do not withdraw on their own, surgery may be required. In any situation after the patient should follow the recommendations of diet and lifestyle, because 50% of cases come back. An exception is surgery: after it, recurrent hemorrhoids occur in only 5% of patients.
diets
The tasks of nutrition are to save a person from constipation, to prevent the development of inflammation. Sources of fiber are included in the diet: vegetables, herbs, fresh fruits. Grains are handled with care, especially rice - they can make stools thick. In addition, they drink more clean warm water: it does not allow feces to melt, it also speeds up the intestinal cleansing process. Simple carbohydrates and sugar should be discarded so as not to provoke inflammation.
Medical therapy
- Laxatives. Preparations that soothe stools and relieve constipation, prevent new mucosal damage. Drink carefully so as not to provoke loss of intestinal muscle tone and diarrhea.
- Candles with anesthesia. Relieve pain from internal hemorrhoids.
- Vasoconstrictor. This is also a local therapy that reduces swelling.
- Anticoagulants. Stop the bleeding.
- Hormonal preparations. They are used topically (injections) for severe inflammation.
Surgical intervention
In the final stage, hemorrhoids require surgery:
- Connection. An instrument is inserted into the anus, which throws a latex ring over the joint and tightens it. The affected area disappears after 3-4 days.
- laser surgery. The procedure with minimal trauma is almost painless, but there are many contraindications to it.
- Classic hemorrhoidectomy. The joints are removed with a scalpel or a special apparatus, which then "sews" the edges of the mucosa. If necessary, the doctor removes the blood clot during the process.
Alternative medicine
The initial stage of external hemorrhoids includes symptomatic therapy:
- Warm baths. They are made with calendula, chamomile, sage. These herbs relieve inflammation, muscle spasm. They sit in the bath for 20 minutes up to 2-3 times a day.
- Compresses. With grated raw potatoes, aloe juice, chamomile decoction, sea oil. Leave on gauze for 30-60 minutes.
prevention
To avoid the question of how to cure hemorrhoids, follow simple rules:
- Move more. When sitting, get up every 1-2 hours for 5-10 minutes. Walk in the fresh air, choose the stairs instead of the elevator, the ability to walk a few meters on foot and not run a car.
- Watch your diet. Eat more plant-based foods, keep your water balance, do not abuse bread and complex carbohydrates - cereals, pasta.























